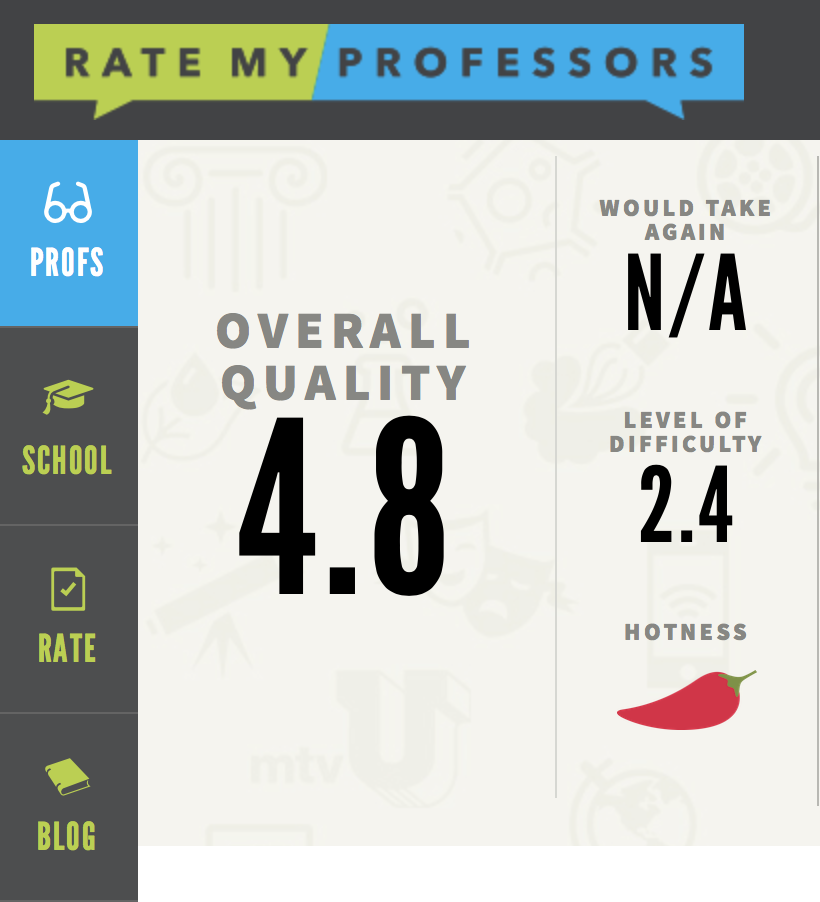
by Dr. Yakov Barton
For decades, we’ve been captivated by the idea that trauma and its effects might be “in our genes.” Early research pointed to genetic predispositions for addiction, depression, and other trauma-related symptoms, suggesting that inherited DNA might carry the weight of generations. But more recent science is telling a more nuanced story—one that shifts the focus from fixed genetic codes to how family dynamics and learned behaviors shape our experiences and responses. In fact, trauma appears to be far more transmitted through nurture, environment, and relational modeling than through genetic inheritance alone.
Genes vs. Epigenetics: A Vital Distinction
While genetics play a foundational role in determining physical traits like eye color or height, their influence on complex psychological patterns like trauma responses is far less deterministic. Instead, epigenetics—the study of how environmental factors influence gene expression—provides a clearer window into how trauma is passed down. Stress, neglect, or other adverse experiences can chemically modify the way genes function, potentially priming someone for heightened stress sensitivity or difficulty regulating emotions. These changes are not permanent but are influenced by the environment and can even be reversed with healing and support.
Yet even epigenetics, for all its insights, is not the dominant force in intergenerational trauma. The most profound transmissions of trauma occur not through altered genes but through how we live, relate, and parent. A child who grows up witnessing a caregiver’s hypervigilance, emotional avoidance, or outbursts of anger often internalizes those patterns, shaping their own relationship to safety, trust, and connection.
The Role of Family Dynamics and Complex Trauma
Trauma’s real legacy is found in the relational dynamics that ripple across generations. Parents who were raised in environments of chaos or neglect may unconsciously model those patterns, not out of malice but because unresolved trauma shapes their emotional availability, boundaries, and coping strategies. Children absorb these dynamics as their blueprint for navigating the world, and the cycle continues. This is particularly evident in complex PTSD (cPTSD), where chronic relational trauma—especially in childhood—leads to long-term emotional dysregulation, self-perception struggles, and difficulties forming healthy relationships.
For years, the role of genetics in behaviors like addiction or depression was overestimated, often leading to a fatalistic view of trauma transmission. While biological predispositions matter, research increasingly shows that environmental and relational factors—what families teach, model, and reinforce—play the far greater role. A child with no genetic predisposition for anxiety, for instance, can still develop hypervigilance if raised in an unpredictable or emotionally unsafe environment. Conversely, a supportive and nurturing family can help buffer even genetically vulnerable individuals from trauma’s effects.
The Opportunity for Healing and Change
The good news is that the transmission of trauma is not inevitable. Because much of what perpetuates trauma lies in relational dynamics, healing can happen relationally too. Therapy modalities like internal family systems (IFS) and somatic approaches like EMDR help individuals recognize and rewire the patterns they’ve inherited. Parents who process their own trauma can disrupt intergenerational cycles by modeling emotional regulation, open communication, and secure attachment for their children.
Understanding trauma as primarily relational rather than genetic empowers us to take action. It shifts the focus from what’s “hardwired” to what can be healed and transformed. By breaking free from outdated ideas about trauma as destiny, we open the door to a future where generations thrive—not because their genes changed, but because their relationships did.